Both narrative and translation are concepts and knowledge practices with long traditions in the humanities that have been integrated into medical discourse during the last twenty years, albeit in distinct ways. The concept of translation has been embraced by the scientific disciplines through translational research, a methodology aimed at ‘translating’ laboratory findings into concrete human applications. It has also been adopted by the evidence-based medicine movement to facilitate the implementation of evidence into practice through so called “knowledge translation” activities, including systematic reviews of clinical studies and clinical guidelines. However, translation has been adopted uncritically in this new context, as the knowledge practices it denotes remain rooted in a scientific paradigm, emphasizing standardization and reproducibility. Medical translation has shown limited engagement with humanities and social science approaches to epistemic, linguistic, and cultural border crossings. The medical adoption of narrative presents a completely different story. The term “narrative” has found a place within the softer realms of medicine, often under the umbrella of medical humanities, where it is used to foreground patient stories and the human elements of medical care. Unlike the medical framing of translation, the use of narrative in this context reflects not only the adaptation of a concept to accommodate different knowledge practices but also the integration of humanistic methods of study, such as close reading and rhetorical analysis.
Narrative medicine was established as a distinct medical subdiscipline in the early 2000s, with a strong institutional foundation at Columbia University in the United States.1 It emerged in response to concerns that biomedicine pays insufficient attention to human subjectivity, and that the rise of specialization and standardization in clinical practice might marginalize the human aspects of care. It challenges a reductionist, fragmented approach to medicine commonly associated with evidence-based medicine and knowledge translation, where reliance on clinical guidelines for state-of-the-art treatments risks reducing clinical care to a formulaic process. As such, narrative medicine is a direct response to a growing concern that the logic driving the translational turn in medicine has become overly dominant, overshadowing the unique aspects of a patient’s life.
Narrative medicine draws on but diverges from broader discussions of narrative theory in its explicit dedication to enhancing healthcare, stressing that “narrative knowledge and skills have the power to improve healthcare by increasing the accuracy and scope of clinicians’ knowledge of their patients and deepening the therapeutic partnerships they are able to form” (Charon et al., 2017, p. 1). One of its defining features is its acknowledgement of “the importance of the emotion and intersubjective relation borne of the telling and listening that occur in any clinical encounter” (Charon et al., 2017, p. 2). Unlike other varieties of narrative theory, Charon and colleagues (2017) describe narrative medicine as consisting of three essential components, or movements, attention, representation, and affiliation, which I discuss in greater detail later in this article:
By attention we mean the state of heightened focus and commitment that a listener can donate to a teller—a patient, a student, a colleague, a friend [...]. Representation, usually in writing but also in visual media, confers form on what is heard or perceived, thereby making it newly visible to both the listener and the teller. And affiliation, which results from deep attentive listening and the knowledge achieved through representation, binds patients and clinicians, students and teachers, self and other into relationships […]. (p. 3)
This framework defines narrative medicine as an inherently collaborative practice, marked by attentive listening, meaningful representation, and the development of new relationships. Its aim is to ensure that the patient’s “secret story” can be elicited and studied in the context of the “impersonal intimacy of the medical relationship” and the “narrative, relational, and interpretive domain” that characterizes the patient-healthcare provider encounter (Goyal et al., 2008, pp. 739, 736).
In what follows, I attempt to demonstrate that a perspective that pits narrative medicine against translational medicine, as implied by narrative medicine’s skepticism of clinical guidelines and other knowledge translation tools, is only one side of the story. Rather than being opposites, these two approaches to healthcare should be seen as mutually interdependent. By contesting the dichotomy of art versus science that sets narrative medicine in opposition to knowledge translation, I aim to show that Charon’s concepts of attention, representation, and affiliation can be evoked to demonstrate a supplementary relation between translational and narrative medicine. The supplement, according to Derrida (1997), is at the same time an addition from the outside to something natural and original, and a compensation for an insufficiency inscribed within the natural origin. Hence, the supplement is both cultural and natural, both external and internal to the phenomenon it supplements. My analysis will show that the narrative, relational, and interpretive domains are integral to translational medicine, defining what makes it truly translational. Beyond the immediate clinical encounter, every step of the translational chain involves narrative elements, though these may be less visible than in patient interactions. My aim is to expand the scope of narrative medicine by delving into the black boxes of narrative encounters obscured by laboratory reports, trials, and guidelines.
Goyal et al. (2008) propose “narrative evidence-based medicine” as an elaboration of the translational medicine approach, and suggest that it can effectively bridge gaps in the translational chain by fostering and enriching transformative bidirectional relationships. They further note that most descriptions of the translational research pipeline focus on the transition from basic research to clinical research (T1) and from clinical research to clinical practice (T2), but often neglect the critical role of individual patient decisions. Without incorporating the essential interactions between patients and informed healthcare professionals (termed T3 in their extended model), which are crucial for ensuring patient adherence and benefiting from healthcare recommendations, the translational research model remains incomplete.
While Goyal et al.’s proposed addition to the translational chain (T3) and their overall approach represent a valuable enhancement to translational research, confining the relevance of narrative interactions to a specific step in the translational chain also narrows its scope. This limitation restricts the processes of attention, representation, and affiliation that are central to the practice of narrative medicine to the clinical encounter—that is, to the direct relationship between clinician and patient, as evident from the authors’ framing of the problem: “What the implementation pipeline model [of translational research] does not do is to address the many necessary and relevant aspects of patients’ own direct involvement in their medical care” (Goyal et al., 2008, p. 734).
Goyal et al (2008) view the patient’s story as “the opening gambit in an iterative process of exchanges through which doctor and patient construct a therapeutic intimacy that extends the reach of the relationship” (p. 737), but it remains unclear how this intimacy actually extends the reach of the doctor-patient relationship. Moreover, it is important to explore how narrative medicine can address processes of attention, representation, and affiliation beyond the bedside encounter. The bedside encounter is just one of several “narrative, relational, and interpretive domains” (Goyal, 2008, p. 736) at play along the translational chain from bench to bedside.
In the following discussion, I will explore how the conceptual framework derived from narrative medicine—specifically the concepts of attention, representation, and affiliation—can enhance our understanding of translational processes beyond mere clinical interactions. I will apply and extend these concepts to analyze a T12 study by Dela Cruz et al. (2023) that investigates how mice can model the reproductive effects of puberty suppression with puberty blockers followed by testosterone, a common treatment for transmasculine youths during puberty. In this research, young female mice were used to simulate the hormone treatments typically administered to transgender males during their transition. At 26 days old, the mice received an implant releasing a hormone blocker (GnRHa) for 21 days, followed by weekly testosterone injections for six weeks. To establish control groups, some mice underwent sham surgeries or received sesame oil injections. The researchers monitored various indicators such as the onset of puberty and hormone levels throughout the study, and changes in body and organ weights post-treatment. Their findings indicated that this hormone therapy did not reduce the count of immature egg cells (primordial follicles) in the ovaries, suggesting that the treatment did not adversely affect fertility potential. Nonetheless, they emphasized the need for further research to corroborate these results.
The study is translational in two key ways: it models a human issue—pubertal suppression followed by gender-affirming testosterone therapy in transmasculine youths—through an experiment with mice, and it positions this experiment with mice as a basis for future research involving human subjects. As such, it exemplifies the bidirectional inference between animal experiments and human research that is characteristic of translational (T1) research. I will demonstrate how applying and expanding the concepts of attention, representation, and affiliation to this study can deepen our understanding of the translational processes involved. These processes, I argue, should be viewed as a complex act of meaning-making rather than a straightforward logical inference.
First, however, I will outline the fundamental principles of the translational turn in medicine in order to set the stage for the analysis and explain how the concept of translation is deployed in the field.
Translation in medicine
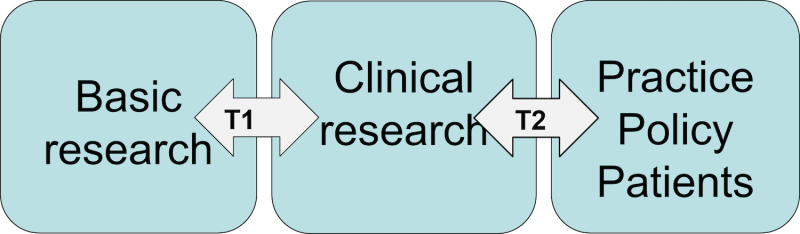
The emergence of the translational turn in medicine in the early 2000s was driven by a growing recognition of the “disconnection between the promise of basic science and the delivery of better health” (Sung et al., 2003, p. 1279). Concerns mounted that despite heightened efforts and investments in research, the returns in terms of improved healthcare were scarce. Traditional methods such as animal experiments, test tube analyses, and early human trials were found insufficient for accurately reflecting patient situations, thus hindering scientists’ ability to predict the efficacy and safety of new treatments or devices (Wehling, 2021). This prompted the need for innovative clinical testing methods that could more effectively bridge the gap between research and treatment. These new methods, collectively referred to as “translational”, were systematically organized into various steps and stages within a sequential process (Woolf, 2008), as illustrated in Figure 1.
Figure 1. The so-called translational chain illustrating translation in two steps (T1 and T2) from basic research via clinical research and into practice, policy, and patient encounters
The first step (T1) involves the transition from basic science to the development and testing of new therapies via clinical trials. The second step (T2) focuses on secondary research needed to convert the results of clinical studies into actionable clinical guidelines. Several variants have since been developed that further elaborate on the details of the pipeline and introduce additional translational steps, all adhering to the same fundamental logic. It is now standard to include a third translational step (T3), similar to that proposed by Goyal et al., that involves translating the guidelines produced in T2 into clinical practice.
While the initial translational step—translational science proper—traditionally received the most attention and funding within the research community, the significance of knowledge translation (KT), which broadens the focus to encompass steps two and three of the translational chain, has grown substantially over the last ten to fifteen years. Whereas the T1 stage is typically viewed in scientific and technical terms, KT is seen as involving adaptation to the behaviour of end users (Davis et al., 2003). It is situated within the larger framework of evidence-based medicine (EBM), which started to emerge in the 1990s and represents a significant transformation in contemporary medicine. EBM challenges the traditional reliance on practicing clinicians’ expertise and pathophysiological reasoning in clinical decision-making, emphasizing the importance of insights derived from ‘objective’, authoritative sources such as randomized controlled trials (RCTs) and systematic reviews of these trials. RCTs are viewed as less susceptible to individual fallibility, compared to the more personalized and potentially biased judgements based on practitioners’ direct interactions with patients and the lived experiences of the latter. EBM categorizes research within a hierarchical structure, with systematic reviews of RCTs situated at the apex, and animal experiments and anecdotal evidence relegated to the lowest tier. Within this framework, KT functions as a transformative process that refines and elevates the body of evidence within the hierarchy, thereby supporting and reinforcing evidence-based medical practices.
Although in principle knowledge translation primarily focuses on how behavioural aspects affect the adoption of research evidence by practitioners and policymakers, it is typically seen as a formal and standardized process, allowing little room for the creativity and productivity we associate with translation in other contexts. The KT framework and the broader EBM paradigm are heavily predicated on the idea that assessing evidence is a highly regimented and mechanistic process. The methodology for assessing knowledge as an integral part of medical decision-making underwent significant standardization towards the latter half of the twentieth century (Timmermans & Berg, 2010). Until the 1950s, the physician personified medical knowledge. They were not mandated to provide any proof of their epistemological authority beyond their professional degree and experience (Weisz et al., 2007). However, mounting skepticism regarding the transparency of individual medical expertise led to the establishment of clinical recommendations through consensus conferences in the 1970s and 1980s. These conferences sought to define clinical directives within specific domains via expert group deliberations. But with the ascendancy of evidence-based medicine, this method was incrementally supplanted by “guideline development”, a process grounded in systematic reviews of randomized controlled trials and evidence grading.
This structure might initially seem paradoxical: laboratory science, typically regarded as the most rigorous scientific component, is perceived as less objective and more susceptible to bias compared to research into actual, less predictable human behaviour in randomized controlled trials. This view is only partially justified. The KT framework acknowledges the scientific validity of claims made within laboratory settings; nonetheless, the ‘truths’ generated are understood to be limited to the specific conditions under which they were created. Consequently, claims deemed strong within the laboratory environment may not necessarily provide robust evidence for specific causal relationships in real-world settings, where they must face different standards for claim validation. The evidence hierarchy could more accurately be described as a hierarchy of commensurability rather than truth. The evidence at higher levels of this hierarchy is intended to be more applicable at the bedside, bridging the gap between controlled experimental conditions and practical clinical application. However, the distinction between commensurability and truth is often subtle and poorly defined within the KT and EBM literature.
I would argue that this lack of clarity and the paradox it engenders result from a failure to reflect on the role of narrativity in the translation of knowledge. In KT, stories are often reductively viewed as a lesser form of discourse, positioned at the bottom of the evidence hierarchy. However, narratives are much more than just a discourse or a code; they function as a meta-code (White, 1980) and a paradigm (Fisher, 1987), representing both a philosophical standpoint and a method for interpreting and assessing human communication. Fisher (1984) defines narratives as “symbolic action—words and/or deeds-that have sequence and meaning for those who live, create, or interpret them” (p. 2). According to Charon (2006), “the engine of narrative is its urge to make sense of why things happen” (p. 48). Our perceptions of the world and the ways in which we assess communication are inherently context-dependent: different interpretive settings, such as the laboratory and clinical environments, generate distinct principles for organizing events and crafting narratives. Within these narratives, varied protagonists and plots emerge, reflecting different fundamental values about truth and validity. The evidence produced in laboratories is not less valid than that from clinical studies; rather, it is of a different nature and involves different key players. Consequently, the connection between the bench and the bedside is not merely a matter of logical inference but also of differing meanings generated in different settings and involving different narrators. This raises critical questions about methodological commensurability: how can we establish shared expectations regarding what constitutes valid procedures for knowledge production across these different contexts?
What I suggest is that we need to reframe the question of how we grade evidence in narrative terms: rather than asking which type of knowledge is more valid, we might ask which is most meaningful in a given context. This approach highlights the potential for engaging with important interactions between KT and narrative medicine that remain unexplored.
Narrative in medicine: Rethinking attention, representation, and affiliation
Charon (2006) defines narrative medicine as “medicine practiced with the narrative competence to recognize, absorb, interpret, and be moved by the stories of illness” (p. vii). A clinician recording a patient’s history, much like a skilled reader analyzing a literary work, must go beyond merely inputting data; they must also capture the patient’s way of conveying their experience, including setting, narrative voice, tone, figurative language, and chronology. Where does the narrative begin? What details are omitted? What perspectives are included, and what are excluded? Furthermore, how do the storyteller and the listener collaboratively construct meaning—and what are the structure and ethics of this interaction (Spencer, 2016)? This close reading approach is further developed into a more elaborate theory that defines “different movements within clinical telling and listening”, as outlined by Charon (2006, 2017). As summarized earlier, these movements consist of attention, representation, and affiliation. Attention, a form of focused listening and understanding, is enhanced by the listener’s effort to re-present what has been heard, often through writing. Both processes foster a stronger affiliation between the teller and the listener, strengthening the bond between doctor and patient and improving diagnosis and treatment.
Despite its potential for broader application, the theory and practice of narrative medicine remain closely linked to the clinical encounter. The concepts of attention, representation, and affiliation situate the narrative framework within human-to-human interactions, highlighting the relational aspect of healthcare. Furthermore, the focus on close reading emphasizes the importance of individual stories, ensuring that each patient’s unique experience is recognized and understood. This approach reinforces the intimate nature of clinical care, enhancing empathy and the therapeutic relationship. At the same time, however, it can sometimes limit the broader applicability of narrative medicine. As Butchart and Parsa (2024) point out, narrative medicine is often too entrenched in traditional literary analysis, potentially overlooking wider social and scientific contexts. Its focus on close reading can be restrictive, limiting its impact to just the interaction between the reader and the text. Despite Charon’s focus on personal encounters, her reliance on literary theory paradoxically tends to emphasize individual texts, which risks neglecting the broader narrative context of healthcare (Butchart & Parsa, 2024).
Rather than seeing this restrictive focus as a limitation inherent to the close reading method, I would argue that it is possible and desirable to apply this approach to stories beyond the bedside context and to narratives that extend beyond individual texts. This clearly requires a revision and expansion of the current understanding of narrative within narrative medicine, a topic I now turn to, focusing on the three pillars of attention, representation, and affiliation. It is worth noting that surprisingly little has been written about the intersection of narrative medicine and knowledge translation (KT), particularly how the narrative competencies described in Charon’s framework—attention, representation, and affiliation—can be effectively applied to KT activities.
Rethinking attention
Attention—or close reading, which serves as narrative medicine’s methodology—is the most developed of the three competencies described by Charon (2005, 2017). In this area, Charon draws extensively on a rich tradition of scholarship within literary theory and narratology, which she meticulously details in her writings. The narrative medicine approach to close reading possesses several distinct characteristics.
To begin with, while Charon (2017) identifies various types of stories as relevant to narrative medicine, including “a novel, a lyric poem, or a paper in JAMA” (p. 165), the primary focus remains on personal stories narrated by individuals within the clinical encounter. This emphasis is further strengthened by the explicit parallels drawn between close reading and attentive listening, which foster intimacy between the narrator and the listener: “This sequence in the office is not unlike a sequence of close reading. The same alert, creative presence is needed by the reader or the listener; the same attention to all features of the narrating are [sic] awakened; the same intimacy between creator and receiver of the narrative is achieved” (Charon, 2017, p. 167).
Charon also distinguishes this type of close reading from the kind of “technical or information-seeking reading” typical of EBM. Close reading in narrative medicine “absorbs a text, squandering nothing” and “thickens and complicates the effects of the words” (Charon, 2017, p. 164). Her approach to reading—or attention, in terms of the proposed three-part movement—also demands narrative humility and an “awareness of the impossibility of knowing accurately what another’s account fully encompasses” (Charon, 2017, p. 173). This perspective on narrative leans towards an aesthetic conception of the text: “The text is treated as a thing of beauty, an occasion of bliss, a created object of both rare delicacy and raw power” (Charon, 2017, p. 165).
Charon’s perspective on close reading is valuable and offers a rich alternative to the purely technical approach to text typical of knowledge translation, especially in relation to interactions between patients and healthcare professionals (a realm described as T3 research by Goyal et al., 2008, within the translational medicine paradigm, as noted earlier). Nevertheless, it remains limited in application and calls for a broader understanding of and a more critical stance towards narrative. Specifically, the close association between narrative medicine and clinical encounters tends to privilege narratives as inherently personal (rather than public, or conceptual) and inherently beneficial to all parties, but primarily to the patient. While the need for critical approaches is recognized by Charon et al. (2017), their depiction of attention as a competency also appears to lack a clear strategy for handling ambiguities, misunderstandings, and conflicts of interest.
In contrast to the clinical context, where the primary goal is to acknowledge the experience of patients and their concerns, an extended definition of KT that engages with its narrative dimension would require a critical close reading approach that pays attention to ambiguities, differences, and misunderstandings in how medical messages are conveyed and the narratives they elaborate. As Misak (2008) asserts, we can learn something important from narrative evidence, but only if we take narratives to be subject to critical scrutiny.
Many scholars in narrative medicine acknowledge the complexity and polyphony of stories. For instance, Frank’s (2013) concept of chaos stories necessarily implies that stories are not always coherent. At the same time, as I already argued, there is a strong association between the story and the individual storyteller in narrative medicine. This link is rooted in the clinical origins of the field, where attention to patients’ stories is understood as part of the healing process. Consequently, the storyteller’s meaning is often privileged, and a lack of coherence in his or her story is conversely often seen as a symptom of ill health and a call for intervention. The more subtle observation of ambiguities, paradoxes, and processes of signification is compromised by the binary division between “ill” and “healthy”, and attention is drawn to the story of the person in need of help. Even as the field has expanded, analysis of the individual storyteller’s narrative still implicitly nurtures the notion of coherence as a given. As a result, the tapestry of stories and ongoing narrative productivity involved in science communication and translation are typically overlooked.
What is needed is an expanded view of narrative that not only encompasses modes of discourse but also ways of thinking—the very form of rationality that informs particular types of narration. Fisher (1987) contends that storytelling is a defining feature of humanity that shapes individuals’ worldviews and influences their interpretation of knowledge and experience. He distinguishes between scientific rationality, which views the world as “a set of logical puzzles that can be solved through appropriate analysis and application of reason conceived as an argumentative construct”, and narrative rationality, which sees the world as “a set of stories that must be chosen among to live the good life in a process of continual recreation” (Fisher, 1987, pp. 59, 8). This means that all knowledge, including scientific knowledge, is shaped as stories and is processed by the human mind as elements within a broader narrative that reflects human values. This idea is encapsulated in the statement that “whatever is taken as a basis for adopting a rhetorical message is inextricably bound to a value—to a conception of the good” (Fisher, 1987, p. 107). Similarly, Misak (2010) argues that value judgements, and therefore narrative rationality, are intrinsic to evidence-based medicine:
But note what is involved in making a strong inference from “treatment T has worked in 90% of the cases for population A” to “it will work in 90% of cases in other populations”. What is required is sound and careful attention to features of the experimental set-up. Judgement is a critical part of a good RCT [randomized controlled trial].
Indeed, judgement is everywhere. Horton notes that we have to judge the applicability of the trial data to the next patient, and Ansari et al. note that “Since guideline development involves an assessment of the overall quality of evidence and complex balancing of trade-offs between the important benefits and harms of any given intervention, arbitrariness, value judgements, and subjectivity ultimately come into play in the guideline development process and associated recommendations”. These are the very things about which EBM is suspicious—assessment, arbitrariness, subjectivity, weighing and balancing, and value judgement. (p. 394)
No evidence is self-interpreting. It is not the evidence alone that determines truth, but rather what we do with the evidence—how we critically assess and deploy it. This critical assessment is the essence of any process of knowledge translation, though it is not often recognized as such.
Walter Fisher’s narrative paradigm offers significant potential for enriching the field of narrative medicine, particularly because it engages with methods of assessing narratives and attempts to elucidate the underlying tension between scientific and narrative rationality. The narrative paradigm sheds light on why individuals might make conflicting decisions about a given issue, even when they agree on the underlying facts. For example, when it comes to prescribing antibiotics for simple infections, doctors—despite having the same training and access to identical guidelines and medical knowledge—might choose different courses of action. This variance in how the evidence is assessed often depends on the doctor’s prioritization of antibiotic stewardship3 versus patient satisfaction and the potential advantages of early intervention in the case of a bacterial infection. The decision can also echo deeper, transcendental values, such as the tension between individual compassion in the face of personal suffering and a collective sense of duty to the broader community. In a similar vein, public decisions about healthcare, like opting for cancer screening or participating in a vaccination program, often depend more on how these choices resonate with an individual’s personal narratives and sense of identity than on a strict adherence to scientific evidence that he or she might not fully grasp at any rate. Fisher’s notion of narrative rationality elaborates these complexities, encouraging a new understanding of knowledge that leads to what he describes as true wisdom.
Traditional rationality, which dominates the field of knowledge translation, evaluates competing narratives based on logical inference, while narrative rationality assesses them based on their coherence and alignment with the audience’s values and experiences. Fisher explains narrative rationality through two analytical principles: probability (the coherence of the story) and fidelity (the credibility of the story for a given individual in a given context). These principles are inherent in our cognitive processes; when we encounter a story, we instinctively assess its probability and fidelity. As readers or listeners, we make sense of a story by asking fundamental questions of probability: Does the story hang together? Is it free of internal contradictions (structural incoherence) and inconsistencies with other stories available to us (material incoherence)? Can it be trusted given what we know about the character of the person delivering the message (characterological incoherence)? The question of probability is inseparable from the question of fidelity: does the story ring true? This is where the reader’s or listener’s response to the text based on their own values comes into play. Whether a text makes sense depends not solely on the text itself, but on the interaction between the text and the reader/listener. We continually assess stories based on other narratives we know and believe in. Elsewhere, Mona Baker and I (2022) have analyzed in detail how this distinction explains differing responses to issues like wearing face masks or observing the rules of lockdown during the COVID-19 crisis. While many people rejected these measures due to what they perceived as encroachments on personal freedom, others accepted them willingly and considered adherence to them a matter of moral responsibility towards others. These mechanisms of assessment are operative, more or less explicitly, in all situations involving the use and translation of any kind of knowledge.
In the article about puberty blockers, briefly introduced above, the text narrates two distinct stories. The first centres on human beings who pursue medical therapy as part of their transition to their affirmed gender. The second story involves mice that are implanted with puberty blockers—a GnRHa depot4—followed by testosterone to study the reproductive effects of blocking pubertal progression followed directly by gender-affirming hormones. The sequence of the two narratives is markedly different. The first is a story of human agency and choice, of “transgender and non-binary people” who “seek medical therapy as part of their transition to their affirmed gender” (Dela Cruz et al., 2023, p. 257). The second involves animals “implanted” to suppress pubertal progression, ultimately leading to their “sacrifice” (Dela Cruz et al., 2023, p. 258). The two stories rest on an inherent assumption of a fundamental difference: humans possess the right to choose, a right that animals do not have. However, the narrative rationality of these two stories, and their respective underpinning values, are not acknowledged in the study. Instead, the connection between them is treated as a straightforward logical inference grounded in scientific rationality, bypassing the complexities of meaning and the differing values to which the two stories adhere.
Do the stories and the translation between them hang together? To what extent do they ring true to their readers? While some may view such an experiment as a necessary sacrifice to tackle significant social and medical challenges, others might object to the apparent lack of coherence between promoting the freedom and right of human beings to choose their identity, which the experiment aims to support, and depriving animals involved in the experiment of their freedom and rights. At the same time, the probability (i.e., coherence) of each story also depends on its fidelity, in the sense of whether it aligns with readers’ experiences and other narratives in which they believe. Although not acknowledged in the article, moreover, the use of puberty blockers in transgender treatment is a deeply politicized issue. Several countries, including the UK, have recently retracted or banned the use of gender reassignment hormone treatments for minors. One of the arguments supporting this policy was recently articulated by the Canadian conservative politician Pierre Poilievre in an interview with CBS News (Tasker, 2024):
“Puberty blockers for minors? I think we should protect children and their ability to make adult decisions when they’re adults,” Poilievre said.
“I think we should protect the rights of parents to make their own decisions with regards to their children.”
According to Poilievre and those who share his values, protecting children from making the wrong decisions is more crucial than their freedom to choose their identity. Instead of allowing children and young adults to decide, it is the parents’ freedom and right to make decisions on behalf of their children that should be safeguarded.
Cathryn Oakley presents an opposing viewpoint to CNN (Cole, 2023). As the state legislative director and senior counsel for the Human Rights Campaign, one of the largest LGBTQ rights groups in the US, Oakley emphasizes the autonomy of young adults:
“These are people who are old enough to enlist in the military, buy guns, buy alcohol, buy tobacco, get married, do a variety of other things that we leave to adults to do,” Oakley noted. “And yet we would be forbidding them from being able to receive gender affirming care, as if that is in some way a more permanent decision.”
How readers relate to these narratives and their underlying values will likely influence their opinions on the legitimacy of the reported experiment and the ‘sacrifice’ of the animals involved. The primary consideration here is that close attention to narrative rationality—specifically the probability and fidelity (in Fisher’s terms) of the story about the experiment—may be more important than technical discussions about the robustness of its design and execution, which are usually the focus of scientific rationality and traditional knowledge translation. These narrative aspects are vital in assessing whether and how the experiment appears meaningful and trustworthy within its translated context, and should be incorporated in narrative medicine’s definition of attention.
Representation as re-narration
According to Charon (2006), representation and attention are inseparable in the practice of narrative medicine: “Attention will not be achieved and will not work without the obligatory corollary of representation”(p. 137). Drawing on authors and thinkers like Henry James and Paul Ricœur, she emphasizes representation, or mimesis, as a practice: “Mimesis creates something through its praxis, something that was not there before the act” (Charon, 2006, p. 138). Like Ricœur, she views mimesis as a three-stage act: mimesis1 (prefiguration), mimesis2 (configuration), and mimesis3 (refiguration).
The first stage, prefiguration, suggests that we are always approaching the world with certain prior conceptual schemes that are a product of cultural, historical, and personal contexts (Ricœur, 1984). This includes our language, our cultural norms, and our past experiences. Such factors prefigure our perception and interpretation of the world, providing a framework that guide how we understand new information or experiences. In other words, this stage involves all the conditions that make interpretation possible. The second stage, configuration, involves the act of emplotment, where disparate events are woven into a coherent whole, imparting meaning and direction. In the third and final stage, refiguration, the new narrative or reconfigured understanding that emerged from the configuration stage is integrated back into our life world. This integration means that the stories we tell and the interpretations we create begin to inform and reshape both our own perception and understanding of the world, as well as that of our audience. As Ricœur explains, mimesis3 “marks the intersection of the world of the text and the world of the hearer or reader, the intersection, therefore, of the world configured by the poem and the world wherein real action occurs and unfolds in its specific temporality” (Ricœur, 1984, p. 71; cited in Charon, 2006, p. 138).
The relevance of these insights to knowledge translation is clear, though Charon’s focus is primarily on the clinical setting. KT inherently involves retelling, which, as Charon emphasizes with reference to Ricœur's model, is never a straightforward transfer or replication of the original. Drawing on insights from translation studies, Baker (2014) views translation as a process of renarration, which “constructs rather than represents the events and characters it re-narrates in another language” (p. 159). This perspective suggests that it is impossible to step outside of all narratives to clearly delineate their boundaries or how they represent an external reality. We engage with narratives by creating new ones. This view acknowledges that translators—including knowledge translators—are deeply embedded within the narratives prevalent in their context, actively contributing to the evolution, mutation, transformation, and dissemination of these narratives through their translational choices.
One of the narrative features identified by Baker as central to the process of renarration is selective appropriation. Selective appropriation is inherent in all storytelling and is driven by conscious or unconscious evaluative criteria that reflect the storyteller’s narrative location. This process influences decisions on what to include or exclude, and what to emphasize or downplay in the telling of a story, encompassing both the events portrayed and how protagonists are characterized. This is even more evident in translation than in other instances of renarration that do not involve the crossing of a language barrier, be that a barrier between different languages or between varieties of the same language, where a different audience is addressed:
Selective appropriation is at play in every translation and every interpreter-mediated encounter, in part because differences between the resources provided by each language [or language variety] inevitably oblige the mediator to make choices that involve suppressing some elements and foregrounding others. (Baker, 2014, p. 167)
Like inter- and intra-linguistic translation, KT involves translation across language barriers and varieties. But it also involves interaction between other types of sign systems. For instance, in the study of puberty blockers, distinct markers are used to identify the onset of puberty in mice compared to humans:
Puberty is marked by breast development in girls, followed by pubic hair development and menarche (Lopez-Rodriguez et al., 2021). In female mice and rats, puberty onset is characterized by vaginal opening, first estrus, and ovulation […]. (Dela Cruz et al., 2023, p. 257)
Here, the signs compared represent different indicators of what is purportedly the same biological process. Any additional signs that might appear in the mice, apart from those listed, are overlooked. Adding to this complexity is the way the text navigates the translation between social and biological facts. On one hand, the study frames the transition of transgender and non-binary individuals to their affirmed gender as a social process, emphasizing personal identity and choice. On the other hand, the mice model operates on a different logic: identity affirmation is framed as a process tied to biological intervention, which involves modifying biological markers to provoke a change. As such, the study attempts to reconcile a socially constructed understanding of identity with a biologically deterministic model. By acknowledging and analyzing the choices that shape what is emphasized or omitted, altered or preserved in such processes, narrative theory allows us to gain insight into the underlying biases and frameworks that influence our perceptions and understandings of scientific communication.
Affiliation and interests
According to Charon, attention and representation—the latter sharpened by Ricœur’s specific formulation of mimesis as consisting of prefiguration, configuration, and refiguration—culminate in contact or affiliation. She develops this argument by drawing on the work of psychoanalyst Donald Moss, who states that “[c]ontact taken to its limit, is … the sense that no matter what is about to be said, access to the object will not be lost. Without the belief in the safety of such contact, we are burdened with the threat that sectors of mind, if spoken, will lead to abandonment” (Moss, 2001, p. 1318; in Charon, 2006, p. 150). Although this sense of potential abandonment is particularly visible in the clinical context and in sick people’s fear that some things will disrupt the channels of communication if spoken about (for instance, because they are perceived as shameful or undignified), the need for connection is present in all communication, including communication in the context of knowledge translation. KT focuses on establishing connections with new target audiences and fostering belief in the potential for such connections. This is clearly articulated in the conclusion of the article on puberty blockers:
In conclusion, we have described the first mouse model mimicking gender-affirming hormone therapy in peripubertal transmasculine youth. We demonstrate that this model can be used to study the reproductive consequences of GnRHaþT, of which very little is currently known. (Dela Cruz et al., 2023, p. 264)
In other words, one of the key aims of the study is to establish that translation between mice and humans in this area is feasible and not risky—a notion articulated in narrative medicine as “the belief in the safety of such contact” (Moss, 2001, p. 1318; in Charon, 2006, p. 150).
For Charon (2006), the concept of affiliation carries an inherently positive connotation, closely associated with building community: “All of us who read and write in clinical settings are finding that our practices build community—within medical school classes, among team members on hospital units, in the neighborhood health center between pediatric residents and community health workers” (p. 150). From an alternative but complementary perspective, the concept of affiliation can also be explained through the lens of interests. The practices of scientific writing and reading, both in clinical settings and beyond, are fundamentally driven by interests.
Stengers (1997) rejects the idea of science as “the disinterested activity par excellence” (p. 82), and argues that acceptance of the truth value of any claim, whether scientific or otherwise, hinges on its ability to attract interests. This means that the establishment of facts is always mediated by the interests involved in any context. Employing the term in its original Latin sense of interesse, meaning “to be situated between”, Stengers clarifies that interest in her usage does not necessarily imply malevolence or the pursuit of power or control. Interest is part and parcel of scientific activity. Indeed, “a proposition that does not interest anyone is neither true nor false; it is literally part of the ‘noise’ that accompanies scientific activities” (Stengers, 1997, p. 83). In this sense, reality itself is “not what exists independently of human beings, but that which demonstrates its existence by bringing together a multiplicity of disparate interests and practices” (Stengers, 1997, pp. 164–165).
From this perspective, the affiliation created through narrative medical practices is not solely based on safety or experiences of solidarity, as Charon emphasizes, but also on wants and investments—or interests, in Stengers’ terminology. This is especially relevant in the context of KT, where scientific, political, and pharmaceutical interests often converge. Understanding this landscape is crucial for interpreting the study on puberty blockers discussed here. As evident, for instance, in the comments by politician Pierre Poilievre quoted earlier, political interests have influenced the debate. Pharmaceutical interests have also come under scrutiny. For example, in Texas, Attorney General Ken Paxton launched a formal investigation into whether pharmaceutical companies have been promoting hormone therapies to children and their parents without adequately disclosing their potential long-term effects. In a statement to Reuters, he stated: “I will not allow Big Pharma to misleadingly promote these drugs that may pose a high risk of serious physical and psychological damage to Texas children who cannot yet fathom or consent to the potential long-term effects of such use” (Whitcomb, 2022).
Both the pharmaceutical interests and the political interests involved here underscore the fact that translation from mice to humans involves complex processes of affiliation. In this context, the analytical challenge for narrative medicine goes beyond merely fostering relationships through narrative activities without considering the broader context of interests. It necessitates a critical engagement with these relationships to fully grasp their underlying dynamics and political implications.
Towards a translational narrative medicine
Against this background, what translational narrative medicine could offer is a reframing of the question from “what evidence is the strongest?” to “which knowledge is most meaningful in a given context?”. This shift provides a more nuanced lens for analyzing what specific evidence can be utilized for what purpose in which context. By recognizing that different epistemic cultures—here represented by a story of mice and a story of humans—are narratives shaped by distinct protagonists and rationalities, each reflecting unique systems of values, we can foster a more ethically grounded translational practice. This approach moves beyond reliance on scientific rationality and logical inference alone, embracing a broader, value-sensitive narrative rationality.
Attention, including a critical examination of the narratives involved, focusing on their probability and fidelity, can expose the duality of the narrative and the potential conflict in values. In the context of the study on puberty blockers discussed here, this includes the dissonance between promoting disparate sets of values, for instance, the value of individual freedom and the right of children and young adults to choose their identity, which the experiment supports by making it possible for young transgender individuals to exercise this right, and the value of extending the same freedom and rights to the animals involved in the experiment. Ultimately, determining whether the benefits of the study outweigh its harms remains a value-laden question that reflects the reader’s political perspectives, far beyond the confines of the laboratory.
In the context of knowledge translation, representation involves a complex process of renarration that includes prefiguration to shape perceptions and guide interpretation, configuration to weave disparate events into a coherent narrative, and refiguration to integrate this narrative back into our life world. This process necessarily involves selective appropriation, including decisions on what to include or exclude and what to emphasize or downplay within the narrative. Understanding this complex process can lead to the recognition of alternative narratives that can be constructed based on the same set of events. For example, in the study on puberty blockers, a different pattern of selective appropriation might emphasize details about the treatment and reactions of the animals involved, hence giving more weight to the justification for their sacrifice.
Finally, what Charon identifies as affiliation is essential to any KT process. It involves not only establishing new and credible pathways of connection, such as bridging the gap between mice and humans, but also catalyzing diverse interests and investments, intentionally or otherwise. Examples of such dynamics include the pharmaceutical industry’s promotion of puberty blockers and the subsequent political critiques of its interventions.
In addition to supplementing translational medicine with narrative, relational, and interpretive dimensions essential to understanding its full dynamics, I have also argued that integrating narrative medicine into knowledge translation can provide new insights and broaden the scope of its concepts. In this sense, translational narrative medicine can be understood as translational both in its focus and its methodology—thus expanding the scope of translational medicine in terms of its epistemology, and enhancing the applicability of narrative medicine through an expanded model of both narrative and translation.